Diabetes mellitus, commonly known as diabetes, is a group of metabolic disorders and endocrine diseases characterized primarily by high blood glucose or blood sugar levels over a prolonged period. This occurs either because the pancreas does not produce enough insulin or because the cells have developed insulin resistance. There are three main types of diabetes. These are type 1 diabetes mellitus, type 2 diabetes mellitus, and gestational diabetes or high blood sugar levels during pregnancy. This article focuses on discussing the difference between type 1 diabetes and type 2 diabetes.
Type 1 Diabetes vs Type 2 Diabetes: The Difference
General Differences Between Type 1 and Type 2 Diabetes
Diabetes mellitus type 1 or type 1 diabetes is an autoimmune condition in which the adaptive immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreatic islets. This renders the pancreas unable to produce ideal levels of the hormone called insulin. Insulin enables cells to take up glucose from the blood for energy. This type of diabetes was previously called insulin-dependent diabetes mellitus or juvenile diabetes.
Type 2 diabetes or diabetes mellitus 2 involves an initial insulin resistance in which cells become less sensitive to insulin. The pancreas attempts to produce more insulin as an initial workaround but its insulin-producing beta cells can become exhausted over time and lose their ability to produce enough insulin to control blood sugar levels. This type of diabetes was previously called non-insulin-dependent diabetes mellitus and adult-onset diabetes.
The cause of type 1 diabetes is unknown. Several studies suggest that it involves a combination of genetic and environmental predispositions. Specific theories posit that the cause may be due to genetic susceptibility, diabetogenic triggers, and exposure to an antigen. Type 2 diabetes is also generally believed to be caused by genetic and environmental factors. Lifestyle choices like poor diet and conditions like obesity are considered important risk factors.
Difference in Terms of their Respective Pathophysiology
Both type 1 diabetes and type 2 diabetes have different pathophysiology. The pathophysiology of type 1 diabetes centers on the destruction of beta cells in the pancreas. It is important to note that different risk factors can have their distinctive underlying pathophysiological processes that later result in beta cell destruction. An autoimmune response against beta cells is considered the most common risk factor and process involved in beta cell destruction.
The pathophysiology of type 2 diabetes involves insulin resistance occurring primarily within the muscles, liver, and fat tissues. The pancreas increases its insulin production as an initial solution to persistent high blood sugar levels stemming from the inability of cells in relevant tissues to use this hormone properly. However, as this resistance progresses, insulin-producing beta cells become exhausted. This renders them unable to produce enough insulin.
It is important to underscore the fact that not all individuals with some insulin resistance develop type 2 diabetes. This resistance is common in people who are overweight or with lower physical activity. The inability of beta cells to produce enough insulin is a defining factor in this type of diabetes. Type 2 diabetes is essentially a two-pronged problem that involves insufficient insulin production due to beta cell impairment in the setting of insulin resistance.
Similarities and Differences in Management and Treatment
Both type 1 diabetes and type 2 diabetes have several similar signs and symptoms. These include increased thirst, frequent urination, weight loss despite increased hunger, fatigue, blurry vision, and poor healing. Both also share similar complications like heart disease, stroke, neuropathy or nerve damage, kidney failure, foot ulcers, and damage to the eyes. The main goal of managing diabetes is to lessen these symptoms and prevent complications.
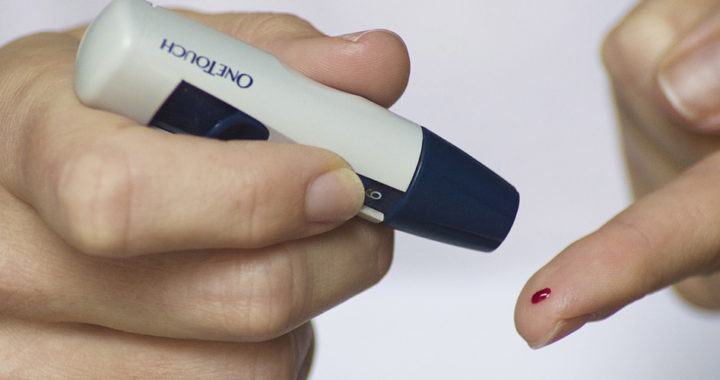
Type 1 diabetes is not preventable. Type 2 diabetes can be prevented or slowed down with diet and other lifestyle modifications. Both also have different management. Type 1 diabetes requires insulin therapy which involves administering insulin via injection. Lifestyle modifications alone are insufficient. Other cases, particularly for type 1 diabetic individuals not responding to insulin therapy, require pancreas transplantation or islet cell transplantation.
Managing type 2 diabetes primarily involves using anti-diabetic drugs like metformin as the first line of treatment. The purpose of these drugs is to increase the amount of insulin produced by the pancreas, increase the insulin sensitivity of targeted organs, or decrease the rate at which glucose is absorbed from the gastrointestinal tract. Some cases may require insulin therapy. Other options include loss programs through diet and exercise or weight loss surgery.
FURTHER READINGS AND REFERENCES
- Akil, A. A.-S., Yassin, E., Al-Maraghi, A., Aliyev, E., Al-Malki, K., and Fakhro, K. A. 2021. “Diagnosis and Treatment of Type 1 Diabetes at the Dawn of the Personalized Medicine Era.” Journal of Translational Medicine. 19(1). DOI: 10.1186/s12967-021-02778-6h
- Lan, Y.-Y., Kovinthapillai, R., Kędzia, A., and Niechciał, E. 2024. “Age-Based Challenges to Type 1 Diabetes Management in the Pediatric Population.” Frontiers in Pediatrics. 12. DOI: 10.3389/fped.2024.1434276
- Quattrocchi, E., Goldberg, T., and Marzella, N. 2020. “Management of Type 2 Diabetes: Consensus of Diabetes Organizations.” Drugs in Context. 9:1-25. DOI: 10.7573/dic.212607